
徐蔚海教授 北京协和医院
世界神经超声联盟神经超声执委会委员
中国医师协会神经内科医师分会神经超声专委会主任委员
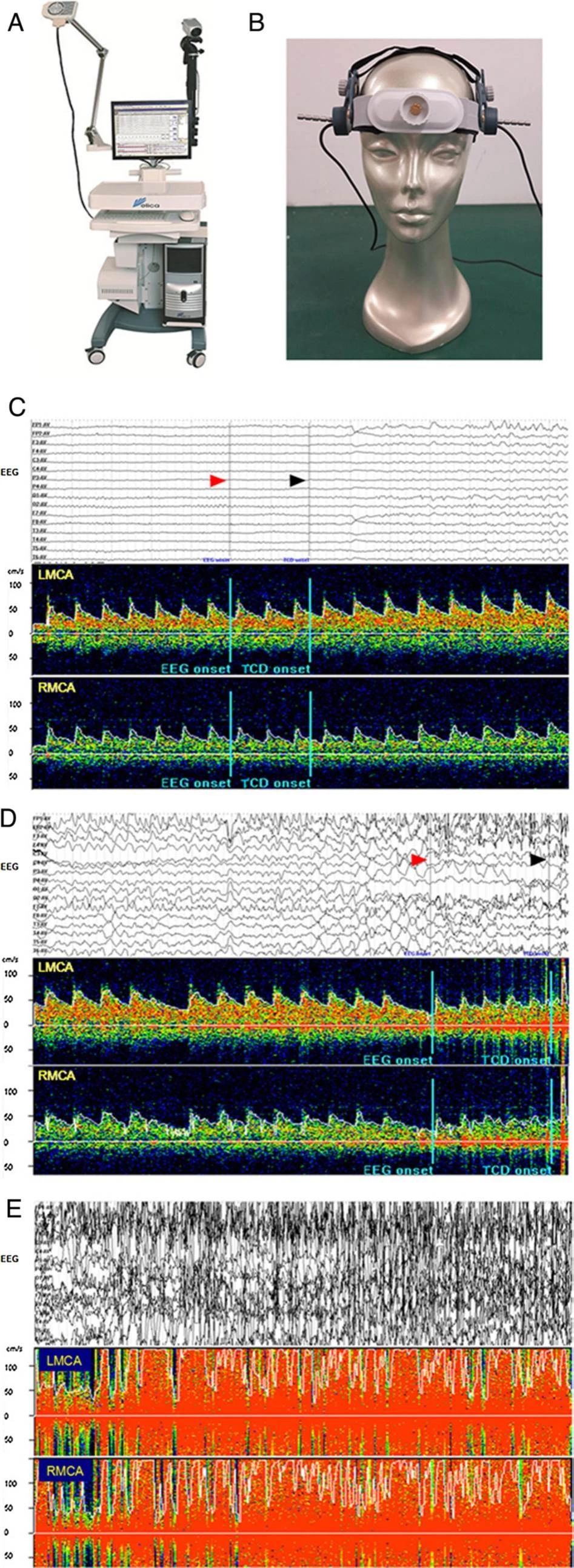
《Real-time TCD-vEEG monitoring for neurovascular coupling in epilepsy》
(Seizure Volume 29, July 2015, Pages 1-3)
【A B S T R A C T】
Purpose: Recently, a novel multi-model monitor has been available, which integrates real-time signals of transcranial Doppler (TCD) and video-EEG (vEEG) 【NSD-8100,Delica,China】into one workstation. We sought to test the feasibility of this device in detecting neurovascular coupling in patients with epilepsy.
Method: Cerebral blood flow velocity (CBFV) of bilateral middle cerebral arteries and vEEG during seizure episodes were recorded simultaneously in 12 patients (age 17–58 years) with partial epilepsies. The correlations between vEEG and CBFV findings were analyzed.
Results: Eleven seizure episodes were detected in 5 patients. Of them, bilateral CBFV increase with interhemispheric asymmetry was observed in 4 seizure episodes of 3 patients. EEG abnormalities preceded CBFV increase by 1–3 s at the onset of a seizure. In a patient with bilateral middle cerebral artery stenosis, no apparent CBFV changes were detected during 2 of 3 seizure episodes. Another patient with previous frontal hemorrhage displayed CBFV increase without interhemispheric asymmetry during 4 seizure episodes.
Conclusion: It is feasible to evaluate neurovascular coupling with good temporal correlation in patients with frequent seizure episodes by real-time TCD-vEEG monitoring.
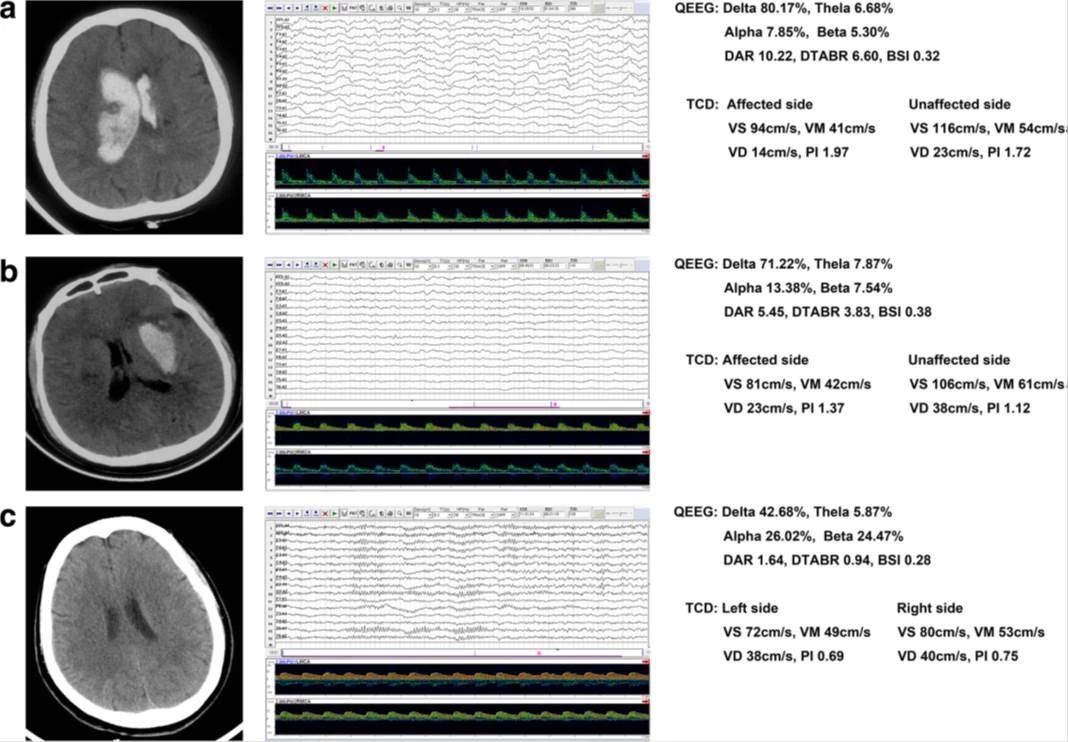
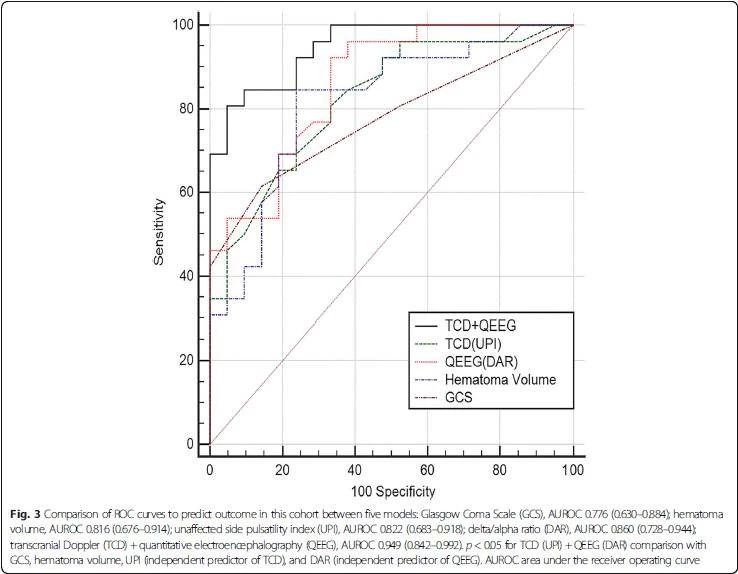
《Transcranial Doppler combined with quantitative EEG brain function monitoring and outcome prediction in patients with severe acute intracerebral hemorrhage》
(Chen et al. Critical Care (2018) 22:36)
【A B S T R A C T】
Background: Neurological deterioration after intracerebral hemorrhage (ICH) is thought to be closely related to increased intracranial pressure (ICP), decreased cerebral blood flow (CBF), and brain metabolism. Transcranial Doppler(TCD) is increasingly used as an indirect measure of ICP, and quantitative EEG (QEEG) can reflect the coupling of CBF and metabolism. We aimed to combine TCD and QEEG to comprehensively assess brain function after ICH and provide prognostic diagnosis.
Methods: We prospectively enrolled patients with severe acute supratentorial (SAS)-ICH from June 2015 to December 2016. Mortality was assessed at 90-day follow-up. We collected demographic data, serological data, and clinical factors, and performed neurophysiological tests at study entry. Quantitative brain function monitoring was performed using a TCD-QEEG recording system at the patient’s bedside (NSD-8100; Delica, China). Univariate and multivariable analyses and receiver operating characteristic (ROC) curves were employed to assess the relationships between variables and outcome.
Results: Forty-seven patients (67.3 ± 12.6 years; 23 men) were studied. Mortality at 90 days was 55.3%. Statistical results showed there were no significant differences in brain symmetry index between survivors and nonsurvivors, nor between patients and controls (all p > 0.05). Only TCD indicators of the pulsatility index from unaffected hemispheres (UPI) (OR 2.373, CI 1.299–4.335, p = 0.005) and QEEG indicators of the delta/alpha ratio (DAR) (OR 5.306, CI 1.533–18.360, p = 0.008) were independent predictors for clinical outcome. The area under the ROC curve after the combination of UPI and DAR was 0.949, which showed better predictive accuracy compared to individual variables.
Conclusions: In patients with SAS-ICH, multimodal neuromonitoring with TCD combined with QEEG indicated that brain damage caused diffuse changes, and the predictive accuracy after combined use of TCD-QEEG was statistically superior in performance to any single variable, whether clinical or neurophysiological。
《颅内动脉重塑研究进展:从局灶性到普遍性重塑》
(中国实用内科杂志 2017 年 11 月第 37 卷第 11 期)
【摘要】
近年来学者们逐渐认识到动脉是一个活跃的器官,会随多种病理生理情况发生重塑。从早期冠心病和周围血管粥样硬化所致的局灶性动脉重塑,到近年来报道的普遍性动脉重塑。文章综述了颅内动脉重塑定义、分类,研究测量方法,重塑机制及与临床症状疾病的关系。
【主要内容】
1、颅内动脉重塑的定义
动脉在不同的生理和病理条件下可向内收缩或
向外扩张,即动脉重塑(arterial remodeling) 。当颅内动脉产生上述现象即为颅内动脉重塑。
2 颅内动脉重塑的测量研究方法
目前动脉重塑的研究大都是横断面研究,难以动态观察病灶处动脉重塑。采用比较斑块处血管管周面积和临近管腔相对正常处血管管周面积的方法来衡量斑块处动脉重塑的情况。
研究者广泛使用重塑率(remodeling ratio,RR) 来判定动脉重塑:RR =病灶处管周面积/ 参照点管周面积;RR>1.05 为扩张性重塑,RR<0.95 为缩窄性重塑,0.95<RR<1.05为无重塑。此测量方法也有一定局限性,由于血管从近端至远端是逐渐变细的,参照点取近端可能会低估RR,参照点取远端可能会高估RR。Qiao等 在矫正了颅内动脉测量点间距离和血管变细的因素后计算了RR。另一方面,在所研究血管可能无法找到完全不受动脉粥样硬化影响的正常参照点。
目前在研究颅内动脉的普遍性重塑上,测量评价方法还没有达成共识。
3 颅内动脉重塑的机制
颅内动脉重塑的机制及病理生理改变还不是十分明确。有限的关于周围动脉的研究表明,血流动力学、 体液因子及炎症与动脉重塑相关。血管内皮接收信号传输给临近细胞,导致一系列影响细胞生长、凋亡、迁移和细胞外基质生成或激活的活动。需要强调的是,在不同的病理生理情况下,参与动脉重塑的主要机制可能是不同的。
4 颅内动脉重塑的临床意义
动脉重塑是决定管腔大小的重要因素。在形态学上,扩张性重塑减轻管腔狭窄,缩窄性重塑加重管腔狭窄。组织学上,扩张性重塑与易损斑块相关,斑块成分有更大的脂质核心、炎症和薄纤维帽;缩窄性重塑与稳定斑块并存,斑块有小的脂质核心和更多纤维等等。
5 总结
动脉重塑是一种常见的在多种生理、病理情况下,血管反应性向外扩张或向内收缩的现象。颅内动脉重塑分为在动脉粥样硬化斑块处的局灶性重塑,及沿整个血管节段的普遍性重塑。关于重塑的病理生理机制和普遍性重塑的研究还很缺乏,需要进一步的研究来系统阐述重塑类型的分布规律及临床意义。研究动脉重塑可能对血管病的病例生理有更深入的认识,对患者个体化精准治疗有潜在意义。
《无症状性基底动脉粥样硬化患者动脉重塑临床研究》
(Chinese Journal of Practical Internal Medicine July 2018 Vol. 38 No. 7)
【摘要】
目的:探究无症状性基底动脉粥样硬化的动脉重塑特征。
方法:回顾性分析北京协和医院2014 年8 月至2016 年12 月前瞻性建立的高分辨磁共振数据库,将基底动脉存在无症状性动脉粥样硬化性斑块的人群和基底动脉正常且未发生供血区缺血性卒中者进行对照研究。采用3D CUBE T1WI 成像方法,测量并比较分析两组人群的斑块和管壁特征,包括管周面积、管腔面积、最大管壁厚度和基底动脉直径。
结果:研究共纳入无症状性基底动脉病变组46 例和对照组55 例。缩窄性重塑是无症状性基底动脉粥样硬化斑块的主要形式,占55.1%。1 例患者的基底动脉可见缩窄性重塑斑块和扩张性重塑斑块共存。与扩张性重塑斑块相比,缩窄性重塑斑块的狭窄率更大(P <0.01),重塑指数、管周面积、管腔面积、管壁面积和基底动脉直径更小(P 均<0.01)。与对照组相比,无症状性基底动脉病变组的基底动脉管周面积和直径差异均无统计学意义(P =0.246,P =0.137),而管壁面积(P <0.01) 和最大管壁厚度(P <0.01) 更大,管腔面积更小(P <0.01)。
结论:无症状性基底动脉粥样硬化存在以缩窄性重塑为主的局灶性重塑,但不存在累及血管走行全程的普遍性重塑。



